- Subclassification of advanced-stage hepatocellular carcinoma with macrovascular invasion: combined transarterial chemoembolization and radiotherapy as an alternative first-line treatment
-
Sujin Jin, Won-Mook Choi, Ju Hyun Shim, Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jinhong Jung, Sang Min Yoon, Jonggi Choi
-
J Liver Cancer. 2023;23(1):177-188. Published online March 23, 2023
-
DOI: https://doi.org/10.17998/jlc.2023.03.04
-
-
1,495
Views
-
88
Downloads
-
3
Citations
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
The Barcelona Clinic Liver Cancer (BCLC) guidelines recommend systemic therapy as the only first-line treatment for patients with BCLC stage C hepatocellular carcinoma (HCC) despite its heterogeneity of disease extent. We aimed to identify patients who might benefit from combined transarterial chemoembolization (TACE) and radiation therapy (RT) by subclassifying BCLC stage C.
Methods
A total of 1,419 treatment-naïve BCLC stage C patients with macrovascular invasion (MVI) who were treated with combined TACE and RT (n=1,115) or systemic treatment (n=304) were analyzed. The primary outcome was overall survival (OS). Factors associated with OS were identified and assigned points by the Cox model. The patients were subclassified into three groups based on these points.
Results
The mean age was 55.4 years, and 87.8% were male. The median OS was 8.3 months. Multivariate analysis revealed a significant association of Child-Pugh B, infiltrative-type tumor or tumor size ≥10 cm, main or bilateral portal vein invasion, and extrahepatic metastasis with poor OS. The sub-classification was categorized into low (point ≤1), intermediate (point=2), and high (point ≥3) risks based on the sum of points (range, 0–4). The OS in the low, intermediate, and high-risk groups was 22.6, 8.2, and 3.8 months, respectively. In the low and intermediate-risk groups, patients treated with combined TACE and RT exhibited significantly longer OS (24.2 and 9.5 months, respectively) than those who received systemic treatment (6.4 and 5.1 months, respectively; P<0.0001).
Conclusions
Combined TACE and RT may be considered as a first-line treatment option for HCC patients with MVI when classified into low- and intermediate-risk groups.
-
Citations
Citations to this article as recorded by  - Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
Journal of Liver Cancer.2024; 24(1): 102. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - How to optimize the treatment strategy for advanced-stage hepatocellular carcinoma with macrovascular invasion
Beom Kyung Kim
Journal of Liver Cancer.2023; 23(1): 121. CrossRef
- Stereotactic body radiation therapy for elderly patients with small hepatocellular carcinoma: a retrospective observational study
-
Jeong Yun Jang, Jinhong Jung, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jin-hong Park, Sang Min Yoon
-
J Liver Cancer. 2022;22(2):136-145. Published online September 16, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.08.18
-
-
2,982
Views
-
73
Downloads
-
5
Citations
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
We aimed to investigate the efficacy and safety of stereotactic body radiation therapy (SBRT) in elderly patients with small hepatocellular carcinomas (HCC).
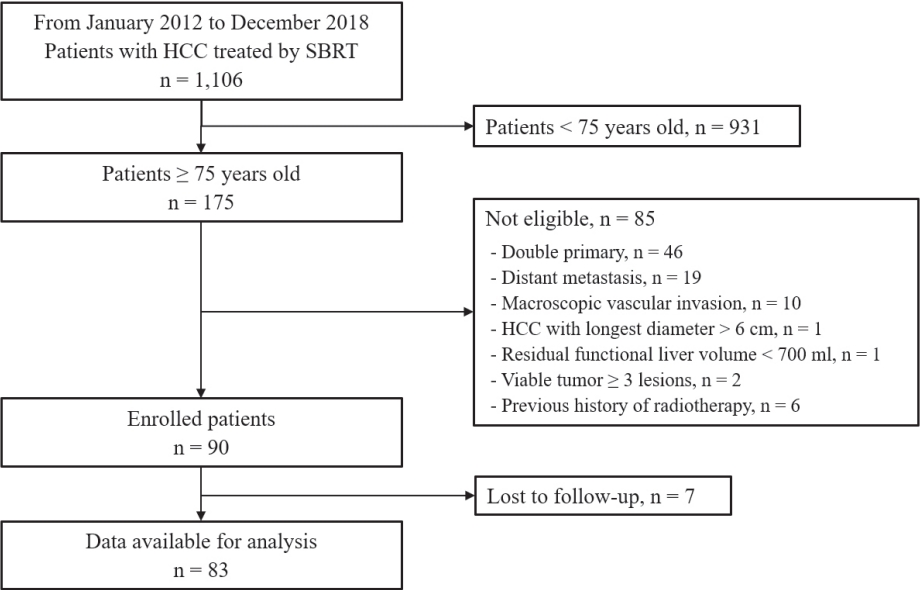
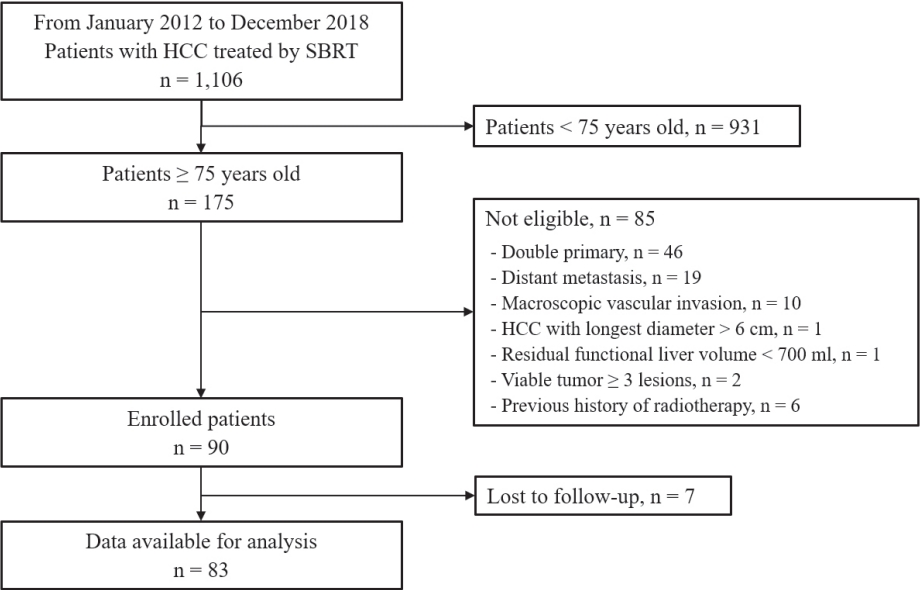
Methods
Eighty-three patients (89 lesions) with HCC who underwent SBRT between January 2012 and December 2018 were reviewed in this retrospective observational study. The key inclusion criteria were as follows: 1) age ≥75 years, 2) contraindications for hepatic resection or percutaneous ablative therapies, 3) no macroscopic vascular invasion, and 4) no extrahepatic metastasis.
Results
The patients were 75-90 years of age, and 49 (59.0%) of them were male. Most patients (94.0%) had an Eastern Cooperative Oncology Group performance status of 0 or 1. Seventy-four patients (89.2%) had Child-Pugh class A hepatic function before SBRT. The median tumor size was 1.6 cm (range, 0.7-3.5). The overall median follow-up period was 34.8 months (range, 7.3-99.3). The 5-year local tumor control rate was 90.1%. The 3-year and 5-year overall survival rate was 57.1% and 40.7%, respectively. Acute toxicity grade ≥3 was observed in three patients (3.6%) with elevated serum hepatic enzymes; however, no patient experienced a worsening of the Child-Pugh score to ≥2 after SBRT. None of the patients developed late toxicity (grade ≥3).
Conclusions
SBRT is a safe treatment option with a high local control rate in elderly patients with small HCC who are not eligible for other curative treatments.
-
Citations
Citations to this article as recorded by  - Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef - Radiotherapy trend in elderly hepatocellular carcinoma: retrospective analysis of patients diagnosed between 2005 and 2017
Bong Kyung Bae, Jeong Il Yu, Hee Chul Park, Myung Ji Goh, Yong-Han Paik
Radiation Oncology Journal.2023; 41(2): 98. CrossRef - Loco-regional therapies competing with radiofrequency ablation in potential indications for hepatocellular carcinoma: a network meta-analysis
Ha Il Kim, Jihyun An, Seungbong Han, Ju Hyun Shim
Clinical and Molecular Hepatology.2023; 29(4): 1013. CrossRef - Has the growing evidence of radiotherapy for hepatocellular carcinoma increased the use of radiotherapy in elderly patients?
Tae Hyun Kim
Radiation Oncology Journal.2023; 41(3): 141. CrossRef - Chronic Liver Disease in the Older Patient—Evaluation and Management
Daniel Anthony DiLeo, Tolga Gidener, Ayse Aytaman
Current Gastroenterology Reports.2023; 25(12): 390. CrossRef
- The effects of immune checkpoint modulators on the clinical course of patients with resectable hepatocellular carcinoma
-
Jihyun An, Hyo Jeong Kang, Eunsil Yu, Han Chu Lee, Ju Hyun Shim
-
J Liver Cancer. 2022;22(1):40-50. Published online March 17, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.03.06
-
-
3,352
Views
-
112
Downloads
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
Immune checkpoint proteins regulating T-cell mediated anti-tumor immunity have been reported to affect clinical outcomes in multiple malignancies. This study aimed to investigate the prognostic effect of histological expression of immune checkpoint proteins in patients with resected hepatocellular carcinoma (HCC).
Methods
A total of 221 patients with HCC who underwent curative resection were included. Expression of programmed-cell death ligand-1 (PD-L1) in tumor cells (tPD-L1) and tumor infiltrating mononuclear cells (TIMCs) (iPD-L1), programmed-cell death-1 in TIMCs (iPD-1), and cytotoxic T lymphocyte antigen-4 in TIMCs (iCTLA-4) were measured immunohistochemically.
Results
Histo-positivity for iCTLA-4, iPD-1, iPD-L1, and tPD-L1 was 32.1%, 42.5%, 35.3%, and 14.9%, respectively. Multivariate logistic analyses revealed that male sex and tumor >5 cm were variables related to iCTLA-4 positivity (odds ratio [OR], 0.46 and 1.94, respectively; P<0.05). Poor differentiation was related to PD-L1 expression in both tumor cells and TIMCs (OR, 2.88 and 3.46, respectively; P<0.05). Microvascular invasion was significantly associated only with iPD-L1 (OR, 2.24; P<0.05). In time-dependent outcome analyses, expression of immune checkpoint proteins in TIMCs (i.e., iCTLA-4, iPD-1, and iPD-L1) was significantly related to longer overall survival and non-cancer-related survival (all P<0.05), but not to time-to-recurrence or cancer-specific deaths. Concurrent activation of the PD-1:PD-L1 and CTLA-4 pathways predicted improved outcomes in terms of overall survival and non-cancer related survival (P=0.06 and P=0.03, respectively).
Conclusions
Immune checkpoint proteins upregulated in TIMCs in HCC tissues have individual and additive effects in prolonging the survival of patients, specifically in terms of survival not related to cancer recurrence.
- A Case of the Effective Treatment of HCC with Bile Duct Invasion and Portal Vein Thrombosis
-
Jihyun An, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2013;13(2):169-172. Published online September 30, 2013
-
DOI: https://doi.org/10.17998/jlc.13.2.169
-
-
 Abstract Abstract
 PDF PDF
- Bile duct invasion of hepatocellular caricinoma (HCC) is rare, ranging from 1.2% to 9%. Moreover, the standard treatment of HCC with bile duct invasion is not yet established. We report a case of HCC with bile duct invasion and portal vein thrombosis which was successfully treated by trasarterial chemoembolization and radiotherapy. A 38-year-old female patient visited our hospital due to right upper quadrant pain. The level of total and direct bilirubin was 6.8 and 4.0 mg/dL, respectively. Her blood test showed HBs Ag positive and the level of alpha-fetoprotein was 43,000 ng/mL. Her CT scan revealed lobulating hypervascular mass involving right hepatic lobe, portal vein and both intrahepatic ducts. We performed endoscopic biliary drainage using biliary stent. She had been diagnosed as HCC on endobiliary biopsy. She was treated with radiotherapy (RT) to portal vein thrombosis, and seven transarterial chemoembolizations. After of all, we carried out radiotherapy to hepatic vein thrombosis and residual HCC near hepatic vein. After the RT, she has been taken care at outpatient clinic without evidence of recurrence during 8 months.
- A Case of Hemolytic Uremic Syndrome after Cisplatin Based Transarterial Chemoembolization
-
Chang Hyeon Seok, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(2):169-171. Published online September 30, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- Hemolytic uremic syndrome (HUS) is a rare condition compromising the clinical triad of acute renal failure, microangiopathic
hemolytic anemia, and thrombocytopenia. HUS may be associated with a variety of etiologies, and chemotherapeutic agents have
also been reported to be associated with HUS, including mitomycin, cisplatin, bleomycin, and most recently gemcitabine. HUS
also has been observed in association with a number of disseminated malignancies in adults, most typically adenocarcinoma of
the stomach and breast. But there was no case report of HUS after cisplatin based transarterial chemoembolization (TACE) for
hepatocellular carcinoma (HCC). We experienced a case of HUS after cisplatin based TACE and reported this case with several
literature reviews.
- A Case of Small HCC
-
Chang Hyeon Seock, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(1):28-31. Published online February 28, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- According to AASLD practice guideline, nodules that are smaller than 1 cm should be followed with ultrasound at intervals
from 3-6 months and nodules larger than 1 cm found on ultrasound screening of a cirrhotic liver should be investigated further
with either 4-phase multidetector CT scan or dynamic contrast enhanced MRI. If the appearances are typical of HCC, the lesion
should be treated as HCC. We experienced a patient who has a hepatic nodule smaller than 1 cm and followed AASLD guideline
and performed radiofrequency ablation for hepatocellularcarcinoma after 13 months later. MRI helped to diagnose hepatic
nodule as a hepatocellularcarcinoma during surveillance.
- A Case of a Advanced Stage Hepatocelluar Carcinoma Patient with Relatively Good Response after Combination Therapy
-
Chang Hyeon Seock, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(1):58-61. Published online February 28, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- According to AASLD practice guideline, for patients who present with advanced hepatocelluar carcinoma, new data indicates
the efficacy of sorafenib in prolonging life. But there are no data comparing combination transarterial chemoemboliation with
sorafenib to sorafenib treatment alone. We experienced a case that treated a patient with combination therapy including
transarterial chemoembolization for intrahepatic hepatocelluarcarcinoma, radiation therapy for portal vein thrombosis and
sorafenib treatment. He was in stable disease state after 6 months later. Therefore, it seems to be need to study for comparing
combination therapy to sorafenib, or to transarterial chemoembolization.
- A Case of Hepatocellular Carcinoma with Bile Duct Invasion Surgically Resected after Transarterial Chemoembolization; Curative Resection after Tumor Downstaging
-
Nae-Yun Heo, Han Chu Lee, Ju Hyun Shim, Kang Mo Kim, Young Suk Lim, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2011;11(1):69-74. Published online February 28, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- A surgical resection is a major curative treatment of hepatocellular carcinoma (HCC) in Korea. However, the respectability of
HCC at the time of diagnosis is low (10-30%) because the cancer is often identified as advanced stage. Nevertheless, some of the
patients were known to have a curative resection after successful downstaging therapy. We report a HCC with bile duct invasion
which was successfully downstaged by the transarterial chemoembolization and treated by surgical resection.
- A Case of Pulmonary Metastasis from Hepatocellular Carcinoma Partially Responsive to Sorafenib
-
Nae-Yun Heo, Han Chu Lee, Ju Hyun Shim, Young-Suk Lim, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2010;10(1):52-54. Published online June 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is one of the most important causes of cancer death in South Korea. Unfortunately, more
than half of the patients are diagnosed in the advanced stage with multiple intra- or extrahepatic metastasis, so no more than
30% of patients are suitable to undergo curative resection. Lung is the most common organ of extrahepatic metastasis of
HCC, and the pulmonary metastasis is known as poor prognosis factor, but no standard systemic therapy is established yet.
Sorafenib is the only molecularly targeted agent which has been proven clinical benefit in the randomized clinical trials, but
pulmonary metastasis is known as predictive factor of poor response. However, we experience a case of pulmonary metastasis
from hepatocellular carcinoma partially responsive to sorafenib, and report it.
- A Case of Advanced Hepatocellular Carcinoma Presenting as Skull Metastasis
-
Nae-Yun Heo, Han Chu Lee, Ju Hyun Shim, Young-Suk Lim, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2010;10(1):73-75. Published online June 30, 2010
-
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma is known to spread to distant organ via hematogenous or osseous route in about 15% of the patients
during its clinical course. However, it is rare that the distant metastatic symptom and sign are the diagnostic clues to find the primary
hepatocellular carcinoma, because most of the patients are likely to expire due to rapid disease progression before the presentation of
the clinical findings of metastasis. Detection of early hepatocelluar carcinoma through surveillance of the high risk population will
reduce the chance of initial presentation of metastatic symptom. In spite of this trend, we experienced a case of hepatocellular
carcinoma presenting as skull metastasis at diagnosis, which suggests that some patients still complain of metastatic symptom as
initial presentation of hepatocellular carcinoma.
- Should We Treat Patients with Massive Hepatocellular Carcinoma? Cons
-
Han Chu Lee
-
Journal of the Korean Liver Cancer Study Group. 2009;9(1):13-16. Published online June 30, 2009
-
-
-
 Abstract Abstract
 PDF PDF
- Massive hepatocellular carcinoma (HCC) is defined as a tumor(s) involving 1 segment or more, with indistinct boundary
in ≥50% of margins. There have been only few studies regarding the treatment response in patients with massive HCC.
Therefore, in this review, the author focused on the treatment response in HCC of ≥10 cm in size. Reported survival rates
after surgical resection are 61~66% at 1 year, 38~44% at 3 years, and 28~31% at 5 years. However, surgical resection is
usually performed in patients with solitary tumor and good hepatic reserve function, and without gross vascular invasion. In
addition, it was reported that surgical complication rate or mortality increases in tumors of ≥10 cm. Therefore, these data
do not represent the outcome after surgical resection in patients with massive HCC. Transarterial chemoembolization (TACE)
can induce objective response in about 65% of patients with HCC(s) of ≥10 cm according to modified EASL criteria.
However, frequent intra- and extra-hepatic metastases are unavoidable and the survival rate was 43% at 1 year and 20% at
2 years. Of note, 11% of cases suffered from serious adverse effects such as renal impairment, sepsis and/or hepatic failure
after TACE. Recently, sorafenib has been shown to increase patient’s survival, but the survival benefit is not still satisfactory.
Other systemic chemotherapies using various combinations of cytotoxic agents usually show 10-20% of objective response,
but there has been no evidence that it can prolong overall patient’s survival. There also has been no evidence that
intra-arterial chemotherapy with or without implantable drug delivery system is superior to conventional chemotherapy or can
prolong patient’s survival. In summary, treatment response in large HCC(s) is not still satisfactory and treatment-related
adverse effects are considerable. Therefore, treatment should be performed in well-selected patients.
- A Case of Hepatocellular Carcinoma with Bile Duct Invasion
-
Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2008;8(1):55-58. Published online June 30, 2008
-
-
-
 Abstract Abstract
 PDF PDF
- Bile duct invasion of hepatocellular carcinoma (HCC) is rare, ranging from 1.2% to 9 %. A 51-year-old male
patient visited our hospital due to jaundice. He had been infected with hepatitis B virus. He had icteric sclera
without abdominal distension or tenderness. The level of total and direct bilirubin was 16.7 and 7.8 mg/dL, each
other. The level of AFP was 4690 ng/mL. CT scan showed ill-defined hypervascular mass involving left hepatic
lobe, left intrahepatic duct and common hepatic duct. He had been diagnosed as HCC on liver biopsy. We
performed total 3 PTBDs in right, left lateral, and left medial side of the bile duct. After then, he was treated with
two transarterial chemoembolizations. Finally, we carried out extended left lobectomy. After the surgery, he has
been taken care at OPD without evidence of recurrence during 8 months.
- Effect of combination therapy with TACE and 3D-CRT for two patients with PVT and/or IVC tumor thrombus
-
Hyun Deok Shin, Young-Suk Lim, Soon Joo Kim, Sang Hyun Park, Gang Mo Kim, Han Chu Lee, Young Hwa Jung, Young Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2007;7(1):87-93. Published online June 30, 2007
-
-
-
 Abstract Abstract
 PDF PDF
- Advanced hepatocellular carcinoma has a poor prognosis, especially in the cases with portal vein or IVC tumor
thrombi. In such cases, surgical resection could not be a curative treatment option and transcatheter arterial
chemoembolization (TACE) alone is usually ineffective. Recently, three-dimensional conformal radiation therapy
(3D-CRT) has been developed to better conform the radiation dose to the tumor volume in order to reach the goal
of eradicating local disease without injuring normal tissue. Combination therapy with TACE and 3D-CRT could
be considered as a treatment option for advanced HCC with PV or IVC tumor thrombi. We report here two cases
with advanced HCC showing response to combination therapy with repeated TACE and 3D-CRT.
- Early Extensive Recurrence of Hepatocellular Carcinoma after Non-surgical Treatment
-
Myoung Kuk Jang, Han Chu Lee, Young-Suk Lim, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2004;4(1):67-72. Published online June 30, 2004
-
-
-
 Abstract Abstract
 PDF PDF
- Although transarterial chemoembolization (TACE) has been reported to have anti-tumor effects in patients with hepatocellular carcinoma (HCC), optimal time schedules and the appropriate follow-up methods have not been determined yet. We experienced a 57-year-old male who underwent radiofrequency ablation(RFA) therapy due to marginal and viable HCC on CT scan after TACE, despite of negative tumor staining on angiography. The patient did not show any evidence of tumor recurrence on CT scan until five months after RFA, However, follow-up CT scan obtained eight months after RFA showed newly developed a massive recurrent tumor with tumor thrombosis in the right portal vein around the previously treated HCC.
- Treatment of Recurrent Hepatocellular Carcinoma After Surgical Resection
-
Han Chu Lee
-
Journal of the Korean Liver Cancer Study Group. 2003;3(1):1-5. Published online July 31, 2003
-
-
-
 PDF PDF
- Outcomes of Liver Resection and Transarterial Chemoembolization in Patients with Multinodular BCLC-A Hepatocellular Carcinoma
-
Jiwon Yang, Won-Mook Choi, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Deok-Bog Moon, Dong-Hwan Jung, Jonggi Choi
-
Received March 3, 2024 Accepted March 25, 2024 Published online April 3, 2024
-
DOI: https://doi.org/10.17998/jlc.2024.03.25
[Accepted]
-
-
 Abstract Abstract
 PDF PDF
- Background
This study aimed to compare the outcomes of liver resection (LR) and transarterial chemoembolization (TACE) in patients with multinodular hepatocellular carcinoma (HCC) within the Milan criteria who were not eligible for liver transplantation.
Methods
We retrospectively analyzed 483 patients with multinodular HCC within the Milan criteria, who underwent either LR or TACE as an initial therapy between 2013 and 2022. The overall survival (OS) in the entire population and recurrence-free survival (RFS) in patients who underwent LR and TACE and achieved a complete response were analyzed. Propensity score (PS) matching analysis was also used for a fair comparison of outcomes between the two groups.
Results
Among the 483 patients, 107 (22.2%) and 376 (77.8%) underwent LR and TACE, respectively. The median size of the largest tumor was 2.0 cm, and 72.3% of the patients had two HCC lesions. The median OS and RFS were significantly longer in the LR group than in the TACE group (p <0.01 for both). In the multivariate analysis, TACE (adjusted hazard ratio [aHR], 1.81 and aHR, 2.41) and large tumor size (aHR, 1.43 and aHR, 1.44) were significantly associated with worse OS and RFS, respectively. The PS-matched analysis also demonstrated that the LR group had significantly longer OS and RFS than the TACE group (PS <0.05).
Conclusion
In this study, LR showed better OS and RFS than TACE in patients with multinodular Barcelona Clinic Liver Cancer stage A HCC. Therefore, LR can be considered an effective treatment option for these patients.
|